What is the EPR?
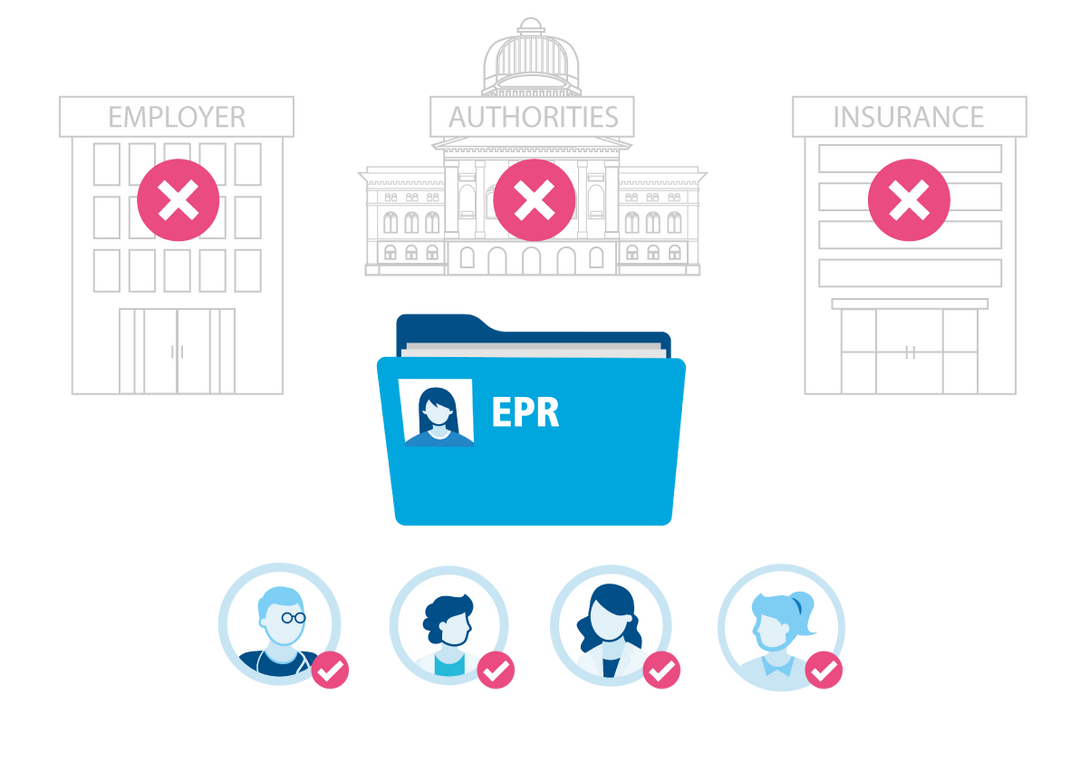
The electronic patient record (EPR) is a collection of personal documents containing information relating to the health of your patients. The patient determines who can see which documents and when. Via a secure internet connection, the information stored in the EPR is accessible to your patients and, if approved, to you as a healthcare professional at any time. This new way of exchanging information between patients and you as a treating healthcare professional is and the foundation for the future of a safe, high-quality and efficient Swiss healthcare system.
The aim of the EPR is set out in the Federal Act on the Electronic Patient Record (EPRA): “The aim of the electronic patient record is to strengthen the quality of medical treatment, improve treatment processes, increase patient safety, enhance the efficiency of the healthcare system, and promote the health literacy of patients.”
.svg)
.svg)
.svg)



.svg)